Working Upstream: Accountable Care Communities
Adam Zolotor, MD, DrPH
President and CEO, North Carolina Institute of Medicine
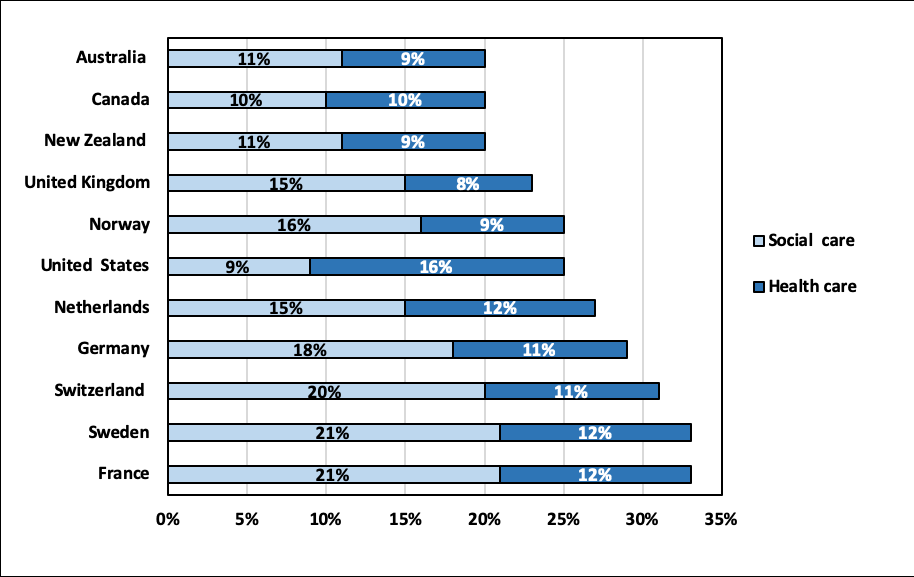
It is clear that health care in the US is the most expensive in the world. We spend nearly twice the percent of our GDP on health care as other industrialized nations—currently at 17.9% of the GDP and climbing steadily to a projected 19.9% of the GDP by 2025. And for all of that investment, we have some of the poorest health with lower life expectancy and higher rates of infant mortality, cancer, heart disease, obesity, and people with two or more chronic conditions than most industrialized nations. One reason is that our system is designed to care for sickness rather than wellness. We spend about twice as much on health care as we do on social care, a ratio that is flipped in most other developed countries (see figure).
Figure: Spending on Health and Social Care as Percentage of Gross Domestic Product in Select High-Income Countries
North Carolina is moving rapidly from a health care system where fees are paid by insurers to providers for services and procedures (office visits, surgeries, etc.) to a system where fees are paid for delivering on wellness. This is known as fee-for-value care and represents a fundamental shift in payment for health care. Between Medicaid transformation and rapid movement in private insurance (Medicare and non-Medicare), we expect that as many as 40% of North Carolinians will have health insurance in a value-based arrangement in the next two years.
This is an incredible opportunity for health systems and communities to re-imagine what we value and why. Health systems will need to deliver on healthy communities and will be paid based on health rather than on procedures. They will need to partner with the communities they serve to identify and pay for appropriate resources (food, housing, transportation, violence prevention, childcare, employment, etc.)
The North Carolina Institute of Medicine convened a task force to develop a model known as Accountable Care Communities (ACCs) in NC (also known as Accountable Communities for Health, Accountable Health Communities, and other names). ACCs are coalitions of cross-sector stakeholders, including health care providers and community agencies that work together to improve health in a community. ACCs integrate health care, public health, education, and social services to address multiple determinants of health, including social determinants. The development of these models is happening alongside the transition to value-based payment systems that put a focus on patient outcomes rather than the amount of health care services provided. An ACC requires a true partnership between human service organizations and health systems with shared risk, shared reward, and shared governance.
Core features of an ACC include:
- Assessment of community health
- Education and advocacy
- Screening tool
- Referral process
- Navigation services
- Tracking system
- Outcomes data and analysis
- Financing plan
- Governance plan
The NC DHHS Healthy Opportunities portfolio and much of the work of county health departments will address many of the core features of an ACC. Many health systems in NC have begun to work with communities to develop some of the features of an ACC and many community coalitions in the state are working toward these goals as well. The ACC model is an ambitious and optimistic set of strategies that are being used to improve the health of communities across the country. These strategies represent a way of thinking about the role of community partnerships in developing a system for health—not sickness.
Dr. Adam Zolotor is the President and CEO of the North Carolina Institute of Medicine and an associate professor of Family Medicine at the University of North Carolina School of Medicine. He is the featured keynote speaker at the Poe Center’s 2019 annual meeting and conferences, WELLNESS: Back to basics.
Featured Poe Event: Wellness: Back to Basics – The Poe Center’s Annual Meeting and Conferences
Date: September 9th-11th, 2019
Time: See event for details

The Poe Center’s 2019 Annual Meeting and Conferences will examine wellness and will focus on the essentials for good living. This three-day event will feature a VIP Event at the Poe Center, a breakfast at WakeMed’s Andrews Center in Raleigh, and a luncheon and panel discussion hosted by the Greensboro College Department of Kinesiology at Mane Stage conference room at Reynolds Family Student Life Center in Greensboro.
Dr. Adam J. Zolotor, President and CEO of The North Carolina Institute of Medicine, Professor of Family Medicine at the University of North Carolina, and this month’s Poe blog contributor will be the featured keynote speaker in Raleigh and Greensboro.
These events will highlight healthy habits and how we can improve individual and community well-being.
Featured Crio Lesson: Stress – How to Deal
Grade Level: K- 5th grade | Program Length: 15-45 min
The Poe Center has partnered with SAS through Curriculum Pathways to provide online access to health science and health education lessons at no cost to teachers across the State of North Carolina. Designed to complement its health education curriculum, the Poe Center’s programs and online content are aligned with the North Carolina Department of Public Instruction’s Healthful Living and Science Essential Standards.
This lesson will describe what stress is, when we might experience stress, and ways we can manage stress including yoga, meditation, and deep breathing exercises. Appropriate for 4-5th grades as a supplemental activity to Decisions…Decisions…